Hyperpigmentation and acne
Hyperpigmentation from acne is a common skin condition that affects many people, particularly those from ethnic groups with darker skin tones. It is characterised by dark spots or patches on the skin, which appear after acne spots have resolved.

What is Hyperpigmentation?
Hyperpigmentation is when the skin produces excess melanin, the pigment that gives skin its colour. When the body produces too much melanin in certain areas of the skin, dark spots or patches will develop. Hyperpigmentation can be caused by a number of other factors, including sun exposure, hormonal changes, and certain medical conditions.
Why does acne cause hyperpigmentation?
Acne is one of the most common causes of hyperpigmentation.
When an acne spot develops, there is inflammation in the skin. Inflammation causes skin cells to produce more melanin in certain individuals. This means that red acne lesions can leave behind dark spots or patches when they heal.
Inflammation can also cause melanin to leak from the top layers of the skin (epidermis) to the deeper layers of the skin (dermis), where pigmentation is not usually found.
This means acne causes more pigment molecules and pushes them deeper into the skin.
When pigmentation occurs following any sort of inflammation, including acne, it is called post-inflammatory hyperpigmentation.
Even mild acne can lead to hyperpigmentation.
Pigmentation from acne can be very distressing. Many of our patients tell us that the pigmentation from acne is more challenging to deal with, both physically and emotionally than the acne that caused it. In addition, even mild acne can lead to pigmentation. This means someone who gets 1 or 2 deep spots a month can suffer from pigmentation that can last much longer.
Who is prone to hyperpigmentation from acne?
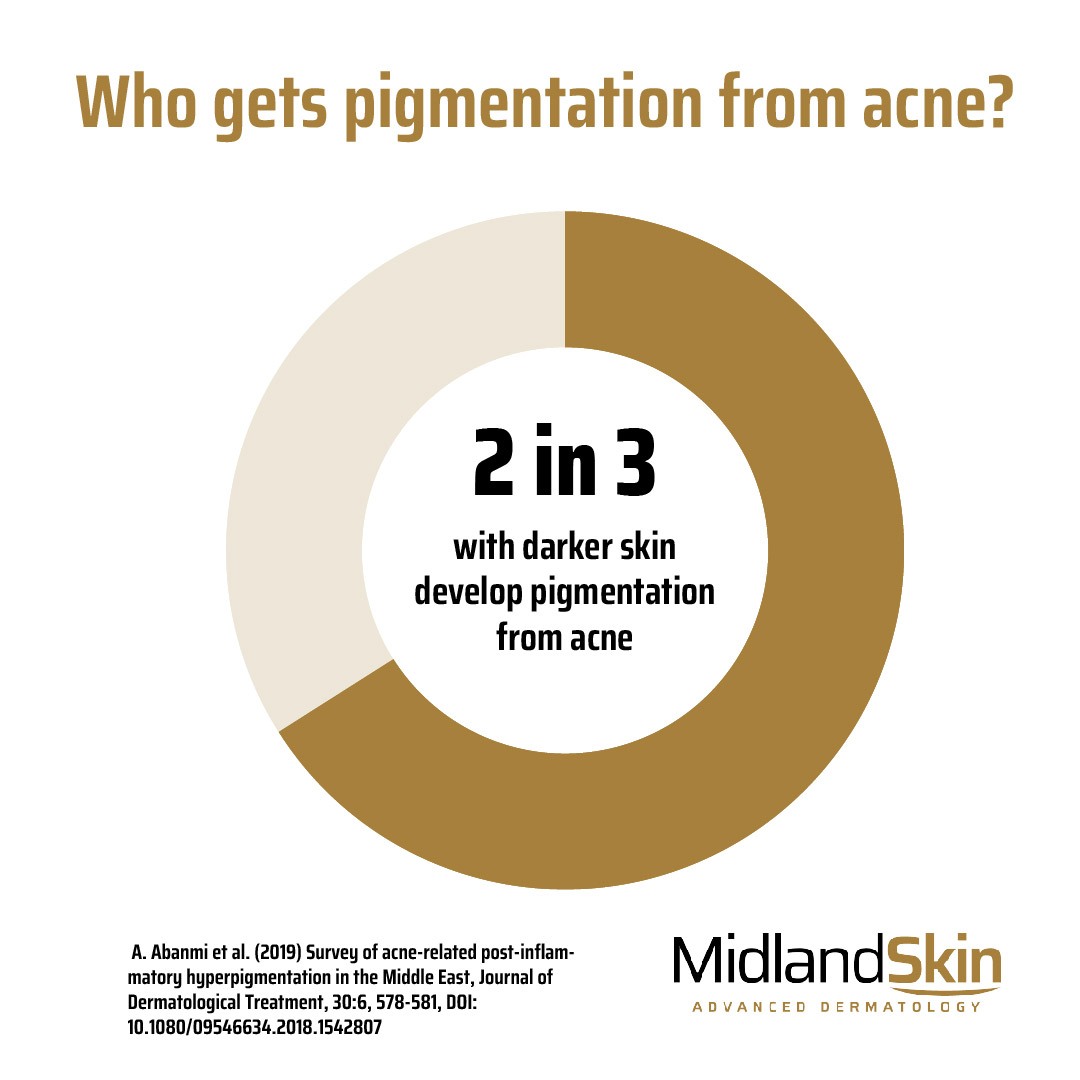
Hyperpigmentation from acne can develop in anyone. Studies have shown that hyperpigmentation from acne can develop in 2 out of 3 people with prone skin types – this means it is a very common problem.
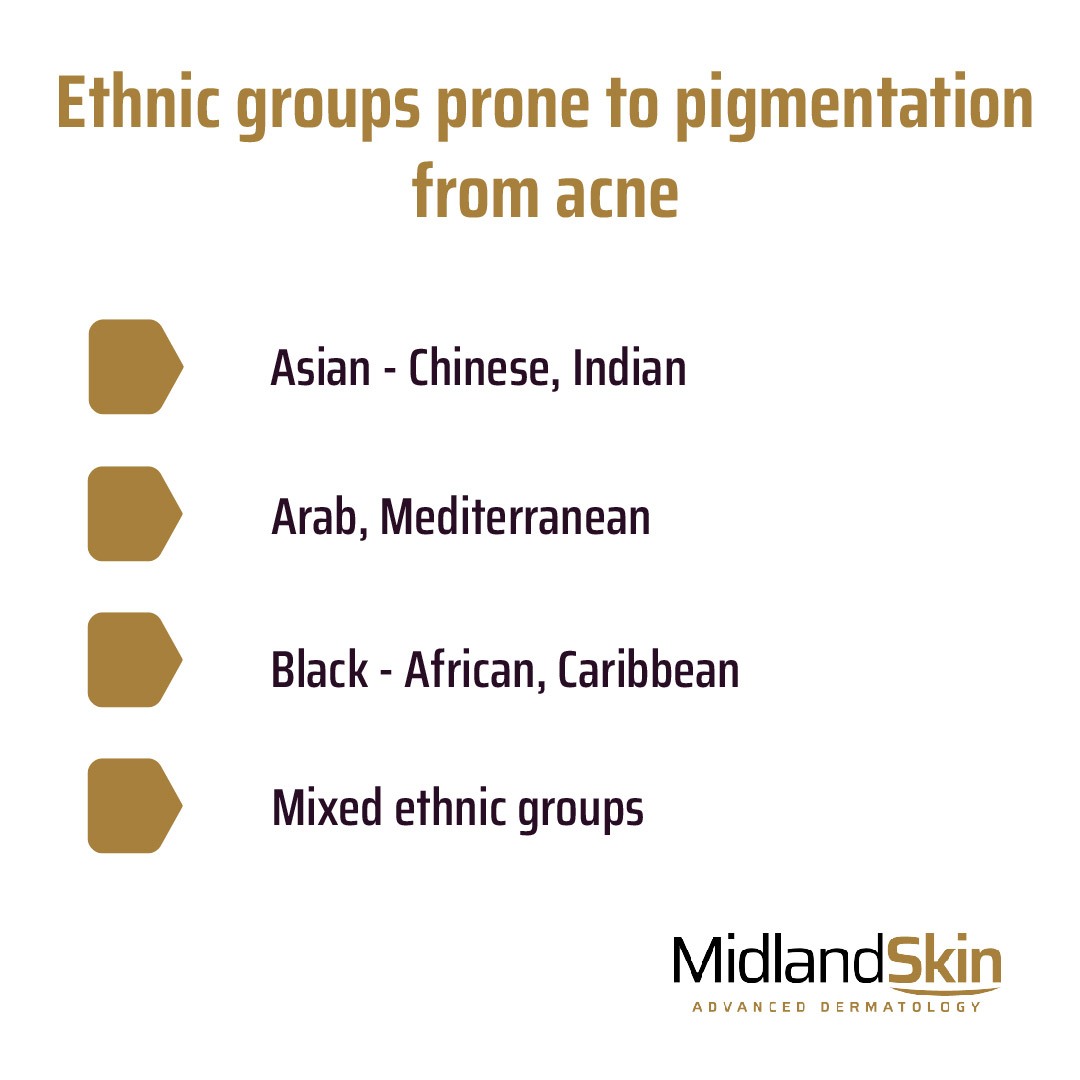
Ethnic groups prone to hyperpigmentation from acne
Ethnic groups with darker skin tones seem to be much more prone. Examples include Asian (Chinese, Indian), Arab, Mediterranean, Black and mixed ethnic groups.
How long does hyperpigmentation from acne last?
The resulting hyperpigmentation can be temporary or longer-lasting, depending on the severity of the acne and the individual’s skin type
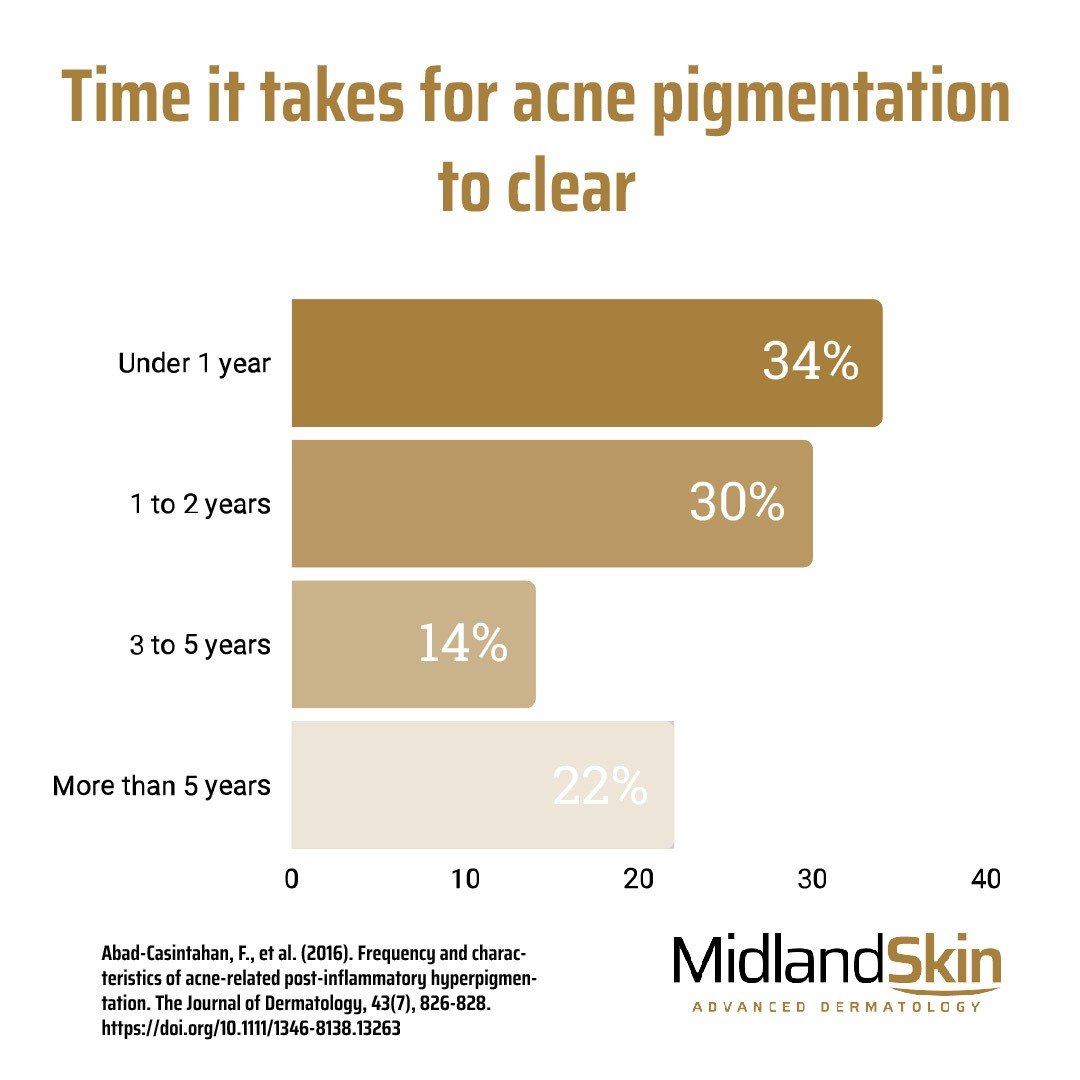
A clinical study from 2016 showed that pigmentation from acne took
- 12 months to clear in 34% of individuals
- 1-2 years to clear in 30% of individuals
- 3-4 years to clear in 14% of individuals.
- Did not clear after 5 years in 22% of individuals
This means that pigmentation can be very long-lasting for some people.
What is the difference between post-inflammatory erythema (redness) and hyperpigmentation from acne?
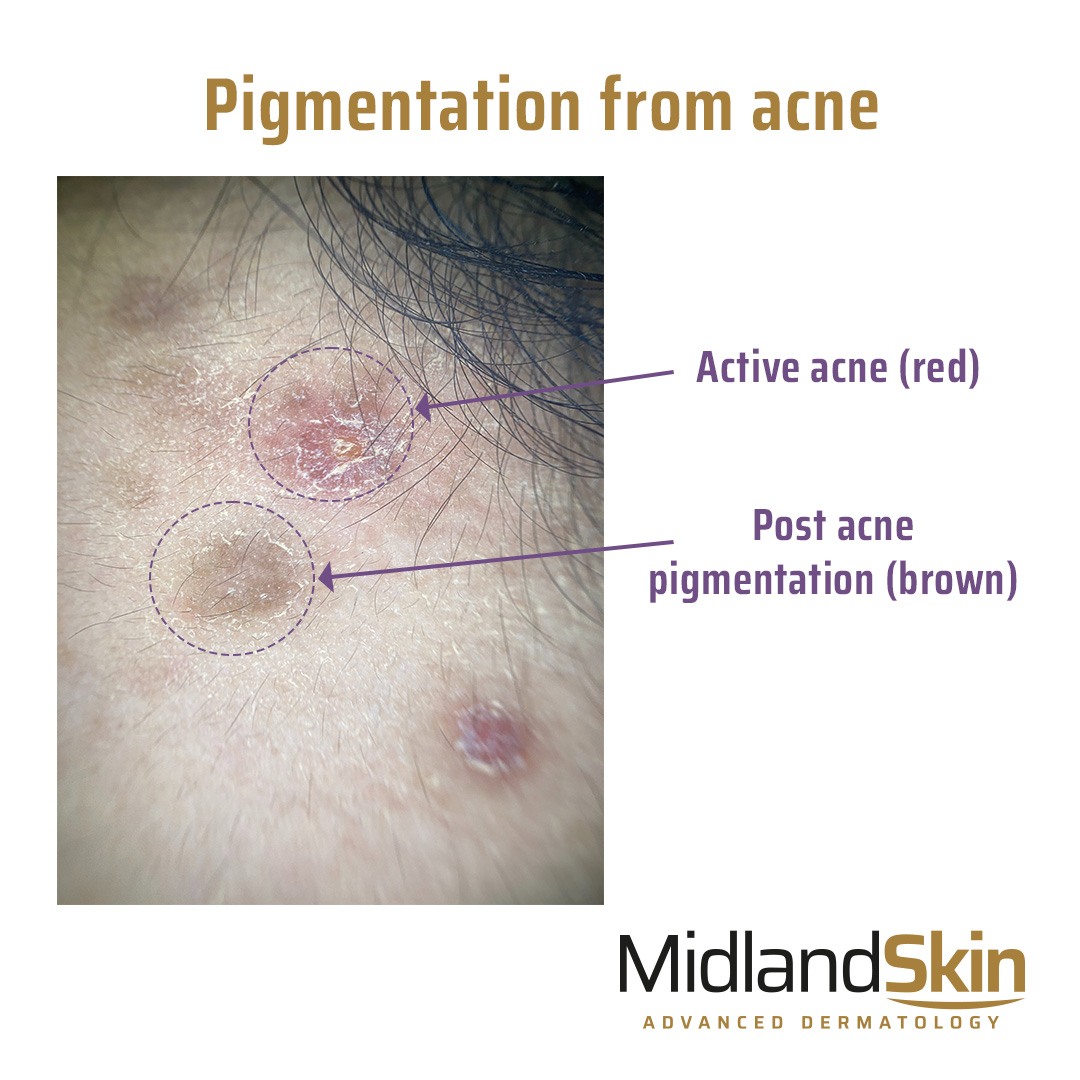
When acne heals, it can also leave red areas that can last several weeks or months. This is because inflammation has caused new blood vessels to form in the skin. This differs from hyperpigmentation from acne, where brown, grey or black pigmented areas develop.
Many individuals have both redness and hyperpigmentation present at the same time.
Post-inflammatory redness is best treated with lasers.
What is the difference between acne pigmentation and acne scarring?
Acne pigmentation and acne scarring are different though it is possible to have both at the same time.
Pigmentation is when there is a colour change in the skin that occurs following acne. However, the skin is still flat.
Acne scarring is when there is a change in the texture or contour of the skin, such as a dip, indentation or pit.
What can you do to reduce post-inflammatory hyperpigmentation?
Treat acne
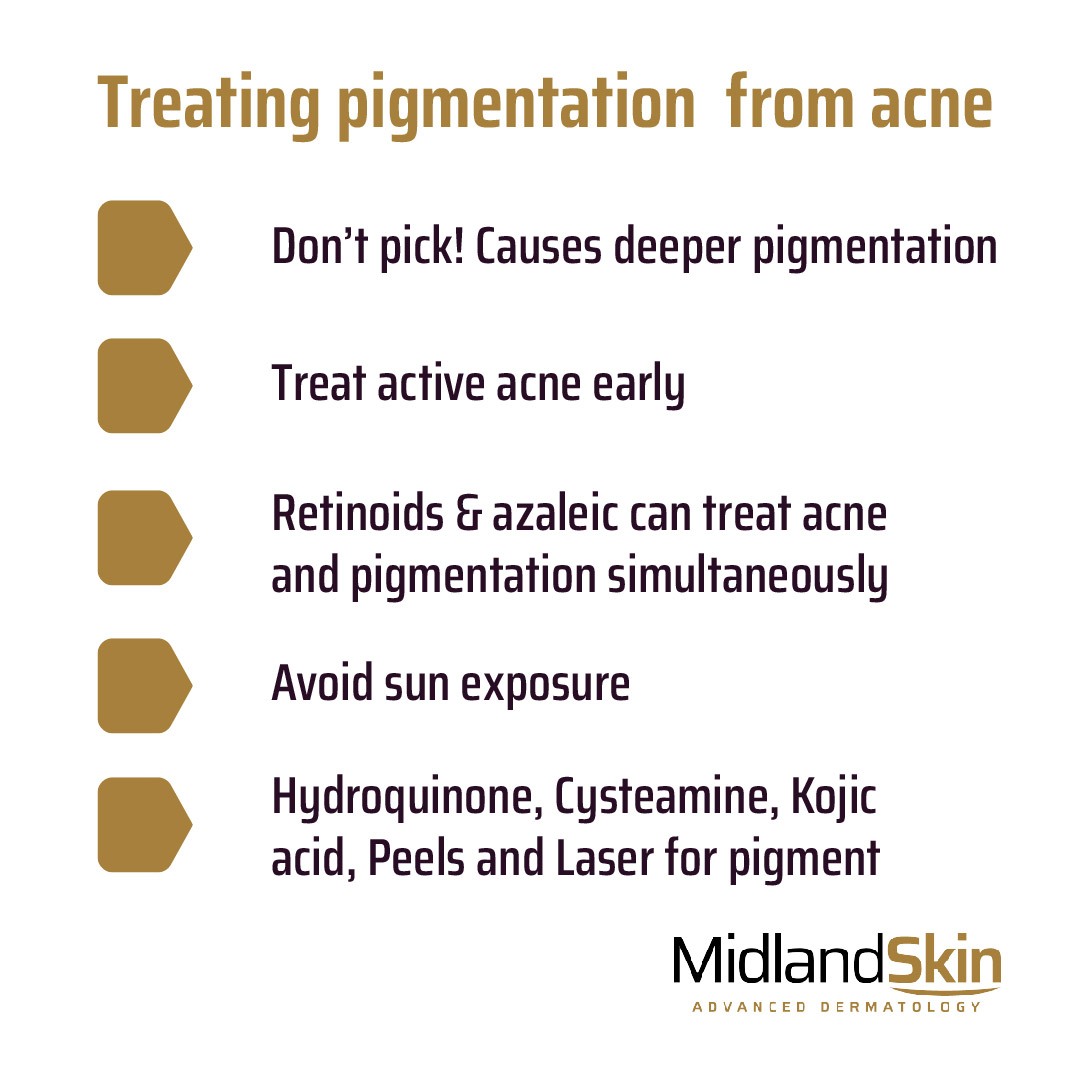
The single most important way to treat pigmentation is to treat the underlying acne that causes it early and properly. This is usually under the advice of a healthcare professional with expertise in managing acne.
Many options are available for treating acne, including prescription creams, tablets and lasers.
RELATED: Acne and acne treatment.
Do not pick
Avoid picking acne as this causes deeper inflammation and worsens pigmentation significantly.
Treatments that clear acne and pigmentation simultaneously
The following treatments improve active acne and target pigmentation simultaneously and may be included in the treatment plan:
- Topical retinoid – especially Tretinoin. Retinoids are great at reducing acne lesions but also reduce melanin production and encourage exfoliation. Link how to use a topical retinoid.
- Azelaic acid – is another ingredient that helps reduce inflammation while reducing melanin production. Concentrations of 15 to 20% are required for best effects.
Additional treatments for pigmentation
Here are some additional ways of reducing pigmentation:
- Avoid the sun. Sunlight stimulates pigmentation, and areas of post-inflammatory hyperpigmentation can darken even further. Therefore you should wear a hat and a factor 50 sunscreen every 2 hours.
- Topical skin-lightening agents. Topical skin-lightening agents, such as hydroquinone and cysteamine, can be used to reduce the appearance of hyperpigmentation. These agents work by inhibiting the production of melanin in the skin.
- Chemical Peels. Chemical peels involve the application of a chemical solution to the skin, which exfoliates the top layer of skin cells to shed away excess pigment molecules. Chemical peels also promote the growth of new skin cells.
- Laser treatments. Laser treatments can be very successful for pigment reduction. This is because lasers work to break down pigment molecules. Different types of laser pigmentation programmes are available depending on the type of acne and individual factors.
What to do next
If you are seeking expert solutions and procedures to reduce hyperpigmentation caused by acne, please contact us to organise an appointment for a consultation.
Author details
Author: Dr Sajjad Rajpar
Date last reviewed: 1 May 2023
Conflict of interest and disclaimer
This information is based on the views of a UK Consultant Dermatologist (a doctor who is on the specialist register for Dermatology, the equivalent of which is ‘Board certified’ in the USA). This information is intended for patients of this Clinic and under our care only. No part of this document should be construed as medical advice. Practices vary nationally and internationally, and we do not wish to contravene advice you have been provided by your own Physician.
References
Abad-Casintahan, F., et al. (2016). Frequency and characteristics of acne-related post-inflammatory hyperpigmentation. The Journal of Dermatology, 43(7), 826-828. https://doi.org/10.1111/1346-8138.13263
Abanmi et al. (2019) Survey of acne-related post-inflammatory hyperpigmentation in the Middle East, Journal of Dermatological Treatment, 30:6, 578-581, DOI: 10.1080/09546634.2018.1542807
Taylor S et al. Treatment recommendations for acne-associated hyperpigmentation: Results of the Delphi consensus process and a literature review. J Am Acad Dermatol. 2023 Mar 15:S0190-9622(23)00366-3. doi: 10.1016/j.jaad.2023.02.053. Epub ahead of print. PMID: 36924935.
Elbuluk N et al. The Pathogenesis and Management of Acne-Induced Post-inflammatory Hyperpigmentation. Am J Clin Dermatol. 2021 Nov;22(6):829-836. doi: 10.1007/s40257-021-00633-4. Epub 2021 Sep 1. PMID: 34468934.

